At the meeting on February 10 I covered the article by Sormanni et al. describing a methodology for computationally designing antibodies against intrinsically disordered regions of proteins.
Antibodies are proteins that are a natural part of our immune system. For over 50 years lab-made antibodies have been used in a wide variety of therapeutic and diagnostic applications. Nowadays, we can design antibodies with high specificity and affinity for almost any target. Nevertheless, engineering antibodies against intrinsically disordered proteins remains costly and unreliable. Since as many as about 33.0% of all eukaryotic proteins could be intrinsically disordered, and the disordered proteins are often implicated in various ailments and diseases such methodology could prove invaluable.
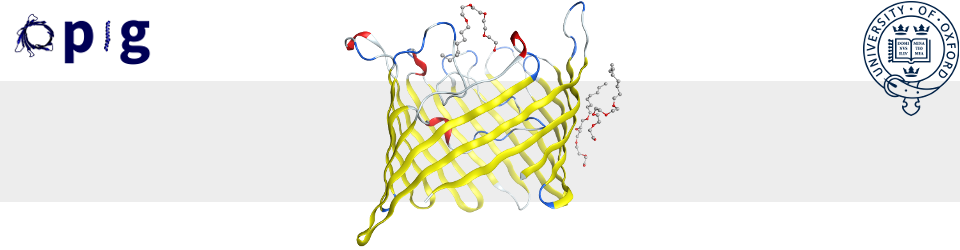
The initial step in the protocol involves searching the PDB for protein sequences that interact in a beta strand with segments of the target sequence. Next, such peptides are joined together using a so-called “cascade method”. The cascade method starts with the longest found peptide and grows it to the length of the target sequence by joining it with other, partially overlapping peptides coming from beta strands of the same type (parallel, antiparallel). In the cascade method, all fragments used must form the same hydrogen bond pattern. The resulting complementary peptide is expected to “freeze” part of the discorded protein by forcing it to locally form a beta sheet. After the complementary peptide is designed, it is grafted on a single-domain antibody scaffold. This decision has been made as antibodies have a longer half-life and lower immunogenicity.
To test their method the authors initially assessed the robustness of their design protocol. First, they run the cascade method on three targets – a-synuclein, Aβ42 and IAPP. They found that more than 95% of the residue position in the three proteins could be targeted by their method. In addition, the mean number of available fragments per position was 570. They also estimated their coverage on a larger scale, using 1690 disordered protein sequences obtained from DisProt database and from measured NMR chemical shifts. About 90% of residue positions from DisProt and 85% positions from the chemical shift could be covered by at least one designed peptide. The positions that were hard to target usually contained Proline, in agreement with the known result that Prolines tend to disrupt secondary structure formation.
To test the quality of their designs the authors created complementary peptides for a-synuclein, Aβ42 and IAPP and grafted them on the CDR3 region of a human single domain antibody scaffold. All designs were highly stable and bound their targets with high specificity. Following the encouraging result the authors measured the affinity of one of their designs (one of the anti-a-synuclein antibodies). The Kd was found to lie in the range 11-27 μM. Such affinity is too low for pharmaceutical purposes, but it is enough to prevent aggregation of the target protein.
As the last step in the project the authors attempted a two-peptide design, where a second peptide was grafted in the CDR2 region of the single-domain scaffold. Both peptides were designed to bind the same epitope. The two peptide design managed to reach the affinity required for pharmaceutical viability (affinity smaller than 185 nM with 95% confidence). Nevertheless, the two loop design became very unstable rendering it not viable for pharmaceutical purposes.
Overall, this study presents a very exciting step towards computationally designed antibodies targeting disordered epitopes and deepens out understanding of antibody functionality.